- 2012年度
- 2011年度
- 新たに判明 がんの転移を促進するメカニズム
(2012/03/23) - 神経発達と加齢における5-hmCを介したエピジェネティクス
(2012/03/23) - TACEを調節するiRhom2は、リステリア菌やLPSの反応により産生されるTNFを制御している
(2012/03/09) - HIV-2って何?
(2012/03/09) - 自殺遺伝子を持ったiPS細胞
(2012/03/09) - リハビリって神経幹細胞も殖やすんです!
(2012/02/24) - 癌幹細胞を制御するHippo pathway
(2012/02/10) - 吸血鬼が若い血を好むのには根拠があった?!~若い生き血でボケ防止~
(2012/02/10) - 癌幹細胞を特異的に標的とした治療法を開発できる可能性!?
(2012/01/27) - 骨の再生には、本来体を守る役割を持つはずのサイトカインは邪魔になる!?
(2012/01/27) - 骨格筋の老化は防げる?
(2012/01/13) - 意外に他力本願???他者の掘ったトンネルを行く癌細胞
(2012/01/13) - 新しいRNA間コミュニケーションのカタチ@筋肉
(2011/12/23) - 精子形成に必須なタンパク質Miwiによるトランスポゾンの発現抑制
(2011/12/23) - Dying well with dementia
(2011/12/09) - Recent insights into the epigenetic regulation of the hair follicle bulge stem cells
(2011/12/09) - ヒトiPS細胞から誘導した神経幹細胞における脳梗塞に対する移植治療の可能性
(2011/11/25) - 体細胞の再プログラム化を阻む"小さなRNA: miR-34"
(2011/11/25) - 薬剤性過敏症症候群 - DIHSがつなぐ薬疹とウイルスとの関連性
(2011/11/11) - 線維芽細胞より作製したドパミン作動性ニューロンは生体内において機能的であるのか?
(2011/11/11) - 終末分化した肝細胞から機能的な神経細胞への直接的な系統転換
(2011/10/28) - Nerves and T Cells Connect
(2011/10/28) - Rapid and robust generation of functional oligodendrocyte progenitor cells
(2011/10/28) - 脂肪細胞が発毛を促進する!?
(2011/10/14) - ADAM13はClass B Ephrinsの分解とWntシグナルの調節により頭部神経冠を誘導する
(2011/10/14) - 多能性の維持に働くchromatin remodeling複合体esBAF
(2011/09/30) - 造血幹細胞の維持にはp57が重要である
(2011/09/30) - IGF-II : 記憶力がよくなる分子!?
(2011/09/16) - 固形腫瘍に存在する間葉系幹細胞は癌幹細胞を増加させる
(2011/09/16) - 小腸は抑制性Th17細胞の宝庫
(2011/09/02) - 細胞周期を制御する新規noncoding RNA
(2011/09/02) - Sema3A play an important role in remyelination failure in multiple sclerosis
(2011/08/19) - Drosophila Sex lethal Gene initiates Female Development in Germline Progenitors
(2011/08/19) - Wnt signaling is a key pathway for regulation of Melanocyte stem cells.
(2011/08/05) - A step closer to understanding the heart
(2011/08/05) - 神経再生を阻む「死」のシグナル
(2011/07/25) - テロメラーゼの再活性化によりマウスの組織老化が回復する
(2011/07/25) - 新遺伝子「Glis1」により、安全なiPS細胞を高効率に作製可能
(2011/07/08) - 幹細胞の"状態"をつくりだす細胞外環境
(2011/07/08) - 毛包幹細胞、色素幹細胞を維持
(2011/06/24) - BCL6を標的とした白血病の新たな治療戦略
(2011/06/24) - 自家移植におけるiPS細胞の免疫応答について
(2011/06/03) - ヒト疾患iPS細胞のウィルソン病への応用
(2011/06/03) - FOP(進行性骨化性線維異形成症)の異所性骨化部の起源は?
(2011/04/22) - 非対称分裂がNotchシグナルの活性化を介して皮膚の分化を促進する
(2011/04/22) - ショウジョウバエの腸管幹細胞の増殖は活性酸素により制御される
(2011/04/22) - 線維芽細胞からの直接的なエピブラストステムセルの誘導
(2011/04/08) - 抗リウマチ薬DHODH阻害剤はメラノーマの進展を抑える
(2011/04/08) - 癌再発の指標になる幹細胞
(2011/04/08)
- 新たに判明 がんの転移を促進するメカニズム
- 2010年度
ホーム > 世界の幹細胞(関連)論文紹介 > Nerves and T Cells Connect
Nerves and T Cells Connect
論文紹介著者

Yan Xiaoxiang(博士課程 2年)
GCOE RA
Department of Cardiology
第一著者名・掲載雑誌・号・掲載年月
Mauricio Rosas-Ballina/Science 2011 Oct 7;334(6052):98-101.
文献の英文表記:著者名・論文の表題・雑誌名・巻・号・ページ・発行年(西暦)
Rosas-Ballina M, Olofsson PS, Ochani M, Valdes-Ferrer SI, Levine YA, Reardon C, Tusche MW, Pavlov VA, Andersson U, Chavan S, Mak TW, Tracey KJ. Acetylcholine-synthesizing T cells relay neural signals in a vagus nerve circuit. Science 2011 Oct 7;334(6052):98-101.
論文解説
Background
Neural circuits regulate organ function in order to maintain optimal physiological stability, providing homeostasis to the body's internal environment. In the immune system, electrical stimulation of the vagus nerve inhibits cytokine release; attenuates tissue injury; and ameliorates inflammation-mediated injury in endotoxemia, sepsis, and other cytokine-dependent models of inflammatory disease. This neural circuit, termed the inflammatory reflex, requires action potentials arising in the vagus nerve, and acetylcholine interacting with the α7 subunit of the nicotinic acetylcholine receptor (nAChR) expressed on cytokine-producing macrophages in spleen.
Electrical stimulation of either the vagus nerve above the celiac ganglion or the splenic nerve itself significantly inhibits tumor necrosis factor-α (TNF-α) production by spleen macrophages, the principal cell source of TNF-α released into the circulation during endotoxemia. Paradoxically, nerve fibers in spleen are adrenergic, not cholinergic, and utilize norepinephrine as the primary neurotransmitter. Thus, although the spleen has been shown to contain acetylcholine, the cellular source of this terminal neurotransmitter in the inflammatory reflex is unknown. Because lymphocytes can synthesize and release acetylcholine, we reasoned that they might be the source of acetylcholine that relays functional information transmitted by action potentials originating in the vagus nerve to the spleen.
Results
- Vagus nerve stimulation increases acetylcholine levels in the spleen.
- Norepinephrine produced by Vagus nerve stimulation significantly stimulated acetylcholine release by spleen lymphocytes.
- Vagus nerve stimulation in WT mice significantly suppressed serum TNF-α production during endotoxemia. Vagus nerve stimulation failed to attenuate serum TNF-α in T cell deficient mice, which indicated that T cell deficiency impairs the inflammatory reflex.
- Flow cytometry analysis revealed that these acetylcholine-producing T cells are CD4+ CD44high CD62Llow memory type T cells.
- Immunostaining showed that acetylcholine-synthesizing T cells in spleen are located in the proximity of catecholaminergic nerve endings.
- Vagus nerve stimulation significantly decreased serum TNF-α levels in endotoxemic nude mice reconstituted with CD4+ CD44high CD62Llow ChAT-EGFP+ cells but not in controls reconstituted with CD4+ CD44high CD62Llow ChAT-EGFP- cells, these results suggested that a subpopulation of helper T cells produced acetylcholine in the spleen and were necessary and sufficient for vagus nerve mediated inhibition of proinflammatory cytokine production.
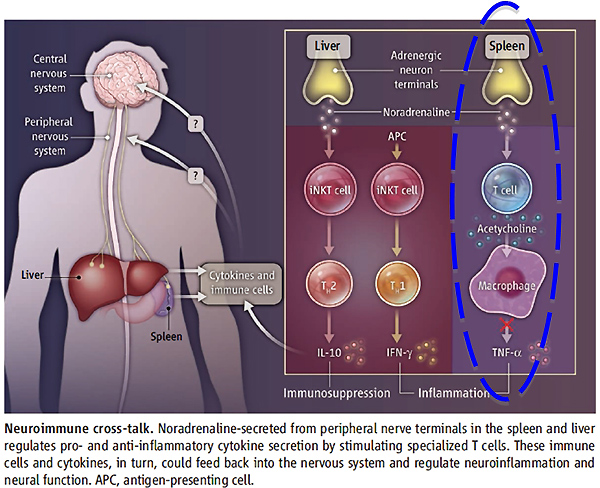
Conclusion: A major finding of this study is the surprising functional role for acetylcholine-producing memory T cells as integral components of a neural information system that controls innate immune responses. It should be possible to target these cells as therapeutic modalities for inflammatory and autoimmune diseases.
用語解説
- ※1 vagus nerve circuit
Copyright © Keio University. All rights reserved.